How to Beat Asthma
The common lung disease debilitates millions of Americans and costs the country billions of dollars, but some very new—and very old—methods are emerging in fighting it.
DENVER, Colorado—I had my first asthma attack in 10 years while working on this story about asthma.
The day had been a grind. I flew to Denver early on a March morning, hoping to give myself a full day to acclimate to the air before I did some jogging and hiking the next day. From the moment I touched down and took a Lyft away from the Denver airport, that unlucky hellhorse, the afternoon was a blur of reporting. At the end of the day, I found some comfort in a bar with some pretty good draught beers and ahi tuna guacamole. Only, the guacamole I ate turned out to be the version with crabmeat. I’m very allergic to crabmeat.
The reaction started mildly enough: a tingling about the lips, itchy arms, and some slightly constricted nasal airways. Nothing a good dose of Benadryl couldn’t fix (Note: I am a bad patient. Epinephrine auto-injectors are the recommended first-line treatments for food allergies). But on the way to the drug store, something deeper kicked in. The coughs to clear my throat became involuntary and more violent, with the whistling rattle of a wheeze. Each breath felt a little less sufficient than the last, and the effort to inhale began to consume me. The recognition of my old nemesis set in, along with that familiar animal panic. I’m having an attack.
I’d come to the Mile High City in search not of situational irony, but of new ways to fight the lung disease that affects me and almost 25 million other Americans, a cohort that has only grown over the past few years. Asthma is one of the most common chronic diseases in the country, and although it rarely kills on its own, it regularly debilitates people, impairs quality of life, and can lead to a lifetime of emergency-room visits and dangerous comorbidities that themselves shorten lives.
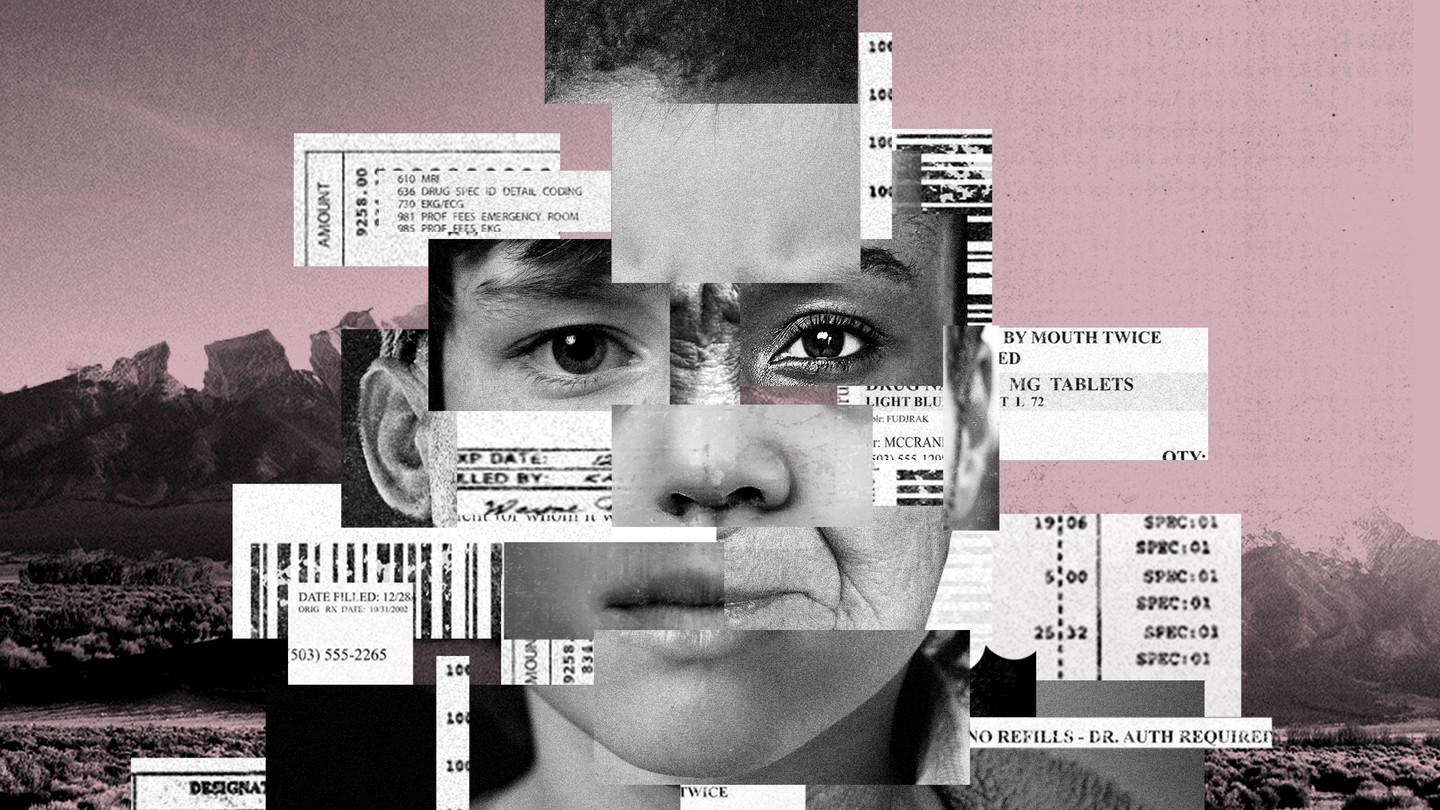
Most people with asthma have at least one attack per year, and the costs compound so much they often destroy households. Asthma costs more than $3,000 per year per person, around $60 billion for the country, and together with COPD it’s one of the five most costly diseases in total. Severe asthma sufferers belong to what we are calling the “platinum patients,” or the five percent of Americans responsible for half of all the country’s health-care costs.
There’s no cure for asthma, but the good news about it is that it can be managed, and the problems associated with it are usually directly linked to that management. Asthma also responds to environmental factors that can be identified and mitigated. There are so many ways that life for asthma patients can be improved without ever needing to visit a doctor’s office that it seems impossible to believe that its devastating effects on human life and its swelling costs can’t be beaten. And some of the most effective therapies don’t necessarily involve medicine at all, but changing the environments in which asthmatics live. For public-health officials, changing the very air people breathe might be the way forward.
* * *
Thus, Denver. The city is a good-enough case study on how to stem the tide of asthma. Metropolises are notoriously bad places for the condition, and existing evidence suggests that factors like air pollution can spur the development of asthma in children, as well as increase the likelihood of attacks among those kids and adults who already suffer from it. Denver’s a bit of a mixed bag. It is among the most polluted cities in America; in the natural bowl created in the shadow of the mountains, air pollution sometimes pools around the city to make an infamous “brown cloud.” And yet Denver’s been in the top 25 of the hundred largest cities in the country for ease of living with asthma for at least the last two years, according to the Asthma and Allergy Foundation of America.
The city performs especially well in several asthma risk factors. One of those factors is the surrounding environment. Although Denver itself faces pollution challenges, people have come to the greater Denver area for at least a century now to escape the symptoms of asthma. Just north of Denver, in Livermore, dozens of kids with asthma go to the American Lung Association-sponsored Champ Camp to hike and canoe through the forests and rivers spilling down from the Rockies, and in the process grow more resilient to attacks. Leaving the city in other directions or heading into the mountains can provide access to some of the cleanest air around.
But even inside the city, there are some unique factors that make coping with asthma easier than a comparable lowland city. In terms of altitude, at least, Denver is the highest major American city, and thus has some of the thinnest air. That might sound like a bad deal for asthma sufferers—and my lungs certainly weren’t too happy my first time jogging the trails in the foothills of the Rockies in nearby Boulder—but an emerging field of research suggests that the altitude and thin air actually can help people with asthma. In fact, a 2016 meta-analysis of that research in the European Respiratory Journal’s Open Research imprint finds that 12 weeks of prolonged exposure to altitudes 1,500 meters or more above sea level can be just as effective in controlling asthma as budesonide, a common long-term asthma-control inhaler. Denver is just north of 1,600 meters above sea level.
Some of the perfect people to ask about altitude and asthma actually work in Colorado. The Institute for Altitude Medicine in Telluride, an old mining town in the San Juan Mountains in the southwest corner of the state, is one of the foremost research centers at the intersection of altitude, human performance, and pulmonology. I called its leading altitude expert Peter Hackett just after touching down in Denver to ask about how the air might benefit me.
“There are dozens of papers about asthma and altitude, and in general asthmatics do better when they go to high altitudes,” Hackett told me. “In fact, if you take urban children and take them to high altitudes for a while, their asthma improves. And if you take mountain kids and send them to an urban environment, their asthma gets worse.” As urban, mountain kids, the effects of altitude in Denver are perhaps limited, but they’d do better in New York than kids from New York.
Nobody knows how long those effects hold for people with asthma who head to high altitudes to gain relief from attacks and then go back to lowland areas. Hackett suggests it might be anywhere from a “few days” to months. But at least some evidence suggests that High-Altitude Climate Therapy, as the concept is known in medical circles, actually changes the immunological profile of asthma sufferers, meaning they not only benefit from reduced allergens at high altitudes, but they become less sensitive to existing allergens. If that evidence holds up, it means the therapy could become part of management routines for people with asthma who live in polluted lowland areas.
In essence, the efficacy of High-Altitude Climate Therapy validates some of the oldest therapies humans have on the books. Fresh air works. As my colleague Julie Beck wrote in reflection on her own hike through the Maroon Bells mountains near Aspen, Colorado, nature therapy is proven for a number of diseases and disorders, including several of the comorbidities like high-blood pressure and heart disease that exacerbate—and are exacerbated by—asthma.
For asthmatics, some of the best respites from the constant fear of attacks might come from finding higher ground, clean air, and perhaps the shade of a grove of non-allergenic alpine trees. There’s a beauty in the thin, crisp, clean air at the top of the world, especially when that air’s always a potential menace, waiting to trigger an attack. For people living in Denver, some of the best natural therapy is just a few miles from the city. But their lives are caught between the natural advantages of living at high altitude and the proliferation of polluting industries in the city.
* * *
Along with the altitude, there’s also some cutting-edge respiratory and allergy science that helps Denver fight asthma. National Jewish Health, located just south of the impressive green spaces and miniature lake at City Park, is consistently one of the best three research-hospital systems in the country for pulmonology. (Interesting footnote: The research center was actually founded by the Jewish service organization B'nai B'rith in 1899 at that Denver location at least in part because of the “good air.”)
A few hours before my ill-fated guacamole encounter, I walked a few miles to National Jewish. Pediatric pulmonologist Tod Olin greeted me with enthusiasm. “I just found out I might get to meet Michael Phelps,” he told me. Turns out, Olympic-level swimmers are abnormally likely to have asthma, and Olin’s research helps train them to cope with attacks, and to even use their familiarity with controlled breathing as an advantage. More applicable to my interests, Olin teaches kids the same lessons and helps them be active.
Olin and a roundtable of his colleagues at National Jewish walked me through how their blend of new science and public-health paradigms can help cut costs and improve asthma care. The first such paradigm is a blurring of the traditional distinction between what’s known as severe refractory asthma—a condition where asthmatics regularly have attacks bad enough to land them in hospitals—and the more mundane variety.
If many or most severe asthma cases can be controlled at home, it would mean a world of difference from a spending standpoint. According to Olin’s colleague Rohit Katial, an allergist and immunologist at National Jewish, “[severe cases] use over 50 percent of all resources,” including dollars spent on care and inpatient days, even though people with severe asthma are in the minority. “That's just because they're going in and out of acute-care settings and emergency rooms, and some of that is just because their disease is bad, and some of it is because they're not in a specialist's hands or can't afford medication, or haven't been educated on the use of their medication.”
But that medication has gotten better, too. Since the advent of steroid-based inhalers, asthmatics have tended towards a generalized treatment of cycling on and off whatever medicine seems to work, and a general avoidance strategy of allergens and triggers. It’s what Michael Wechsler, an adult pulmonologist at the center, calls “a specialist’s art.” But now, they have the technology to make it a science.
“We can start to do personalized analysis now to optimize therapy,” Wechsler told me. Physicians can now blend standard data like age, race, and medical history, along with molecular data like the composition and amount of a person’s eosinophils, a type of white blood cell that mediates asthma attacks. They can also gather extensive epidemiological data on triggers, from dust mites to cockroaches to the exposure to cold air on morning runs. Then physicians can prescribe an exact medical routine, dosage, and trigger-allergen analysis. With that appropriate treatment, wasteful prescriptions, inefficient and ever-changing regimens, and hospital visits can all be reduced, which should dramatically lower how much individuals and the system as a whole spend on health care at a national level.
The science goes even further with some of the secret weapons against asthma that National Jewish researchers helped pioneer. Almost the entire field of asthma pharmaceuticals has relied on steroid-based medicines, for long-term care, and emergency asthma medicine. But for select patients—including several whose asthma doesn’t respond well to traditional management—a new set of therapies called monoclonal antibodies are now hitting the market. These wonder “biologic” drugs, the most popular of which is named Omalizumab, help limit the immune response to allergens and triggers and thus the tendency for asthma attacks, and can actually also help limit asthma attacks even among some sufferers who don’t have a clear allergy trigger.
Wechsler and Katial expressed hope that these medicines would fall in cost as they are subject to more research, and would become more widely available as their need became apparent. If so, along with the rise of personalized medicine and more granular specialist-based care for potentially manageable, the field would be on the brink of revolution. If these new medicines and techniques could cut even half of the spending among the group with severe asthma, that would decrease national spending on asthma by something on the order of $15 billion.
Katial is even more optimistic. He thinks that the existence of biologics and the kind of physiological engineering that can reshape asthma in sufferers might even be able to cure it one day. “Maybe 20 years later, if you’re taking some of these new treatments today, you won’t have attacks,” he told me.
* * *
Of course, it’s never quite that easy. In addition to the often-inescapable pressures of environment and environmental triggers, one of the underlying reasons for the runaway train of dollars spent and years of life lost to asthma is simply access to good care. Scientists and physicians at National Jewish Health aren’t typical of most areas’ asthma medical experts, and according to Olin there are some whole states and several large rural areas that don’t have pediatric pulmonologists at all.
Lisa Cicutto, the director of community outreach and at National Jewish Health, says that so few people with asthma have access to quality medicine and management early on that they often develop lifelong habits that lend themselves to attacks, like inconsistent inhaler use or failing to identify and remove home allergens. “Because asthma is episodic for a lot of people, when they don't have a lot of symptoms and they aren't really bothered by it, they don't want to do anything,” she said. “They're more on the crisis-reactive, as opposed to a crisis-proactive approach.”
Additionally, the ability to manage and effectively maintain asthma regimens are, like just about everything else, connected to income, free time, and the robustness of services in a person’s community. Those measures are in turn directly connected to where people live, the stress they deal with, the amount of environmental degradation they face, and the factors like cockroaches and smog that in turn trigger attacks.
Combined with the stark lack of specialists and services in the poorest places—both urban and rural—there is simply a monumental amount of problems to fix in the communities where asthma hits hardest before any amount of personalized medicine can help. And that’s not counting any potential change in programs like Medicaid that cover most pediatric asthma hospitalizations—changes that might be on the horizon as Congress considers repealing and replacing Obamacare.
The researchers at National Jewish Health have some solutions for those problems, too. For Cicutto, one possible solution to the shortage of health-care providers in poor areas is mobilizing the people who actually serve as first points of contact for kids with asthma: school nurses. “The school nurse is actually seeing the student all the time, and know when they have problems,” Cicutto said. “I consider them the real primary-care providers here.” For Cicutto, arming school nurses or teachers with students’ asthma profiles and training them on how to teach kids about asthma management could be a simple, yet effective strategy.
Currently, the fragmentation of the health-insurance system and medical-privacy laws make such a seamless integration of school nurses and educational professionals into medicine a tricky prospect. But the idea makes sense. If something approaching a tenth of all children will be diagnosed with asthma, and two of the key deficiencies in asthma treatment are management and education, why not emphasize that education in the places they learn everyday?
Wechsler also pointed me to another line of promising policy research. In some cities, policymakers have had success with creatively limiting the exposure of asthmatics to pollution. For example, in Stockholm, Sweden, a “congestion tax” levied by cameras on vehicles in heavy-traffic parts of the city reduced smog and emissions and in turn reduced asthma attacks among kids by as much as 50 percent. One key finding of that experiment is that the main reductions in asthma attacks happened only after a year or longer, which indicates that asthma interventions require patience, and planners and public-health officials have to be in it for the long haul.
These studies and strategies provide some reason for optimism for a way forward. Together, they brought images to my mind of entire communities involved in an integrated asthma-fighting model that treats the home, school, health-care providers, and the environment all as one continuous whole.
One of the worst things about asthma often comes months after an attack. Even for those with insurance, the urgent-care and emergency-room bills, the copays, the costs of tests and overnight stays, the regular cost of upgrading and maintaining asthma devices, and the cost of prescriptions that can often follow severe attacks wreak financial havoc. For people with asthma, these bills are major sources of dread. At worst, they can lead to bankruptcy or other credit disasters.
Add to that the sense of helplessness for people who endure regular attacks, and it’s possible to see how having severe or poorly controlled frequent asthma is a ceaseless cycle of fear. Quite simply, asthma can be a nightmare, even between attacks.
I experienced that nightmare for the first time in years in Denver. Even with insurance, and even in one of the best cities in the world for asthma, with leading asthma researchers at National Jewish ready to for my follow-up call, I was still at the condition’s mercy. But my time hiking around Denver and talking to the foremost experts in the field gave me fresh perspective: With the aid of a blend of personalized medicine, new public-health tools, and new paradigms for deploying these tools, people like me will be more and more likely to be able “to do what they want, when they want, and where they want to do it, and live a normal life,” according to Wechsler.
My last stop in Denver was a salt spa. I’d heard that halotherapy—an alternative-medicine technique where patients sit in a closed cave-like room and inhale aerosolized salt crystals—might be useful for asthmatics. In a touch of irony, the process feels rather like an intensified sensation of inhaling salt spray on coastal beaches, and at least some evidence suggests it might be of some use for asthma, although the overall evidence is mixed for effects on pulmonary diseases.
The spa didn’t do much for me. The air was uncomfortable for me to breathe, and left a tingle in my throat and made my lips dry. I still felt shaky from the previous day’s asthma attack, and unsure whether I should have just scrapped the whole experiment and gone home to order a rescue inhaler for the first time in years.
But, as I sat and inhaled the salt crystals and jotted down my thoughts on the experiment, Tod Olin’s words came to me. “If you look at where asthma was in 1965 versus now,” he’d told me, “lots of people before were basically disabled or worse. Therapies are much better now, and there are so many options to choose from.” The good thing about today is that those options can be as old-school as taking a stroll on a mountain or as advanced as microbiological assays and drugs tailored down to the level of our individual molecules.
And on the horizon, if you squint, perhaps a cure.
This article is part of our project “The Platinum Patients,” which is a collaboration with the Solutions Journalism Network, and is supported by a grant from the Commonwealth Fund.