A longitudinal study of incident hypertension and its determinants in Indian adults aged 45 years and older: evidence from nationally representative WHO-SAGE study (2007–2015)
- 1Department of Health Policy, London School of Economics, London, United Kingdom
- 2Centre for Health and Social Sociences, Tata Institute of Social Sciences, Mumbai, India
- 3Population Research Centre, Dharwad, India
- 4Department of Survey Research and Data Analytics, International Institute for Population Sciences, Mumbai, India
Objectives: Hypertension (HT) is a leading cause of mortality and morbidity in developing countries. This study aimed to estimate the incidence of HT among adults aged 45 years and older in India and its associated risk factors.
Methods: This study used longitudinal data from the Indian sample of the first and second waves of the World Health Organization Study on Global Ageing and Adult Health (WHO-SAGE). A bivariate analysis using Pearson's chi-square test was done to examine the associations of individual, lifestyle, and household characteristics with HT status reported in Wave 2. Incident HT changes were analyzed by adjusting for various covariates in the generalized estimating equation (logit link function) with an exchangeable correlation matrix and robust standard errors.
Results: The study found that during the 8-year period from 2007 to 2015, the incidence of HT in individuals aged 45 years and over was 20.8%. Pre-hypertensive individuals had an overall incidence rate of 31.1 per 1,000 [95% confidence interval (CI): 26.20–35.9] and a 2.24 times higher odds ratio: 2.24 (95% CI: 1.65–3.03) of developing incident HT compared to those who were normotensive. Adults aged 45 years and older, overweight/obese individuals, and women were more at risk of incident HT.
Conclusion: One in five individuals had developed HT over 8 years, with a greater risk of incident HT among women than men. Pre-hypertensive individuals were at a greater risk of developing incident HT compared to normotensive individuals. The study recommends comprehensive and effective management of pre-HT to tackle the burden of HT.
Background
The WHO reported that cardiovascular diseases (CVDs) are the leading cause of death globally, a majority of which occur in low- and middle-income countries (LMICs) (1). Although the prevalence of hypertension (HT) and deaths due to CVDs is on the decline in the developed world, the prevalence is on the rise in LMICs (2). HT is a major risk factor and a leading contributor to premature mortality and morbidity due to CVDs, cerebrovascular events, retinopathy, and chronic renal diseases (3, 4). Globally, an estimated 10.7 million all-cause fatalities in 2015 were related to systolic BP ≥110–115 mmHg, and 7.8 million deaths were related to systolic BP ≥140 mmHg (5).
India—the most populous country with a growing economy (6), an aging population, and increasing urbanization—is also witnessing an increasing prevalence of HT over the years (7) similar to any other LMIC. The United Nations Population Fund projects that the elderly population in India is set to nearly double, reaching a staggering 192 million by the year 2030 (8). A meta-analysis of research conducted between 2001 and 2020 revealed that 24.2% of the Indian population had HT, with 46.8% of those individuals being aware of their elevated blood pressure (9). HT plays a significant role in premature morbidity and mortality in India and contributes to 57% and 24% of all deaths due to stroke and coronary heart disease (CHD) in India (10). Due to demographic shifts, epidemiological changes, and shifts in lifestyle, the prevalence of HT and CVDs in India is projected to increase substantially and is expected to place even greater strain on the healthcare systems of the country that are already under-resourced. The hypertensive Indian population is projected to increase from 20.9% in 2000 to 23.6% in 2025 among women and from 20.6% to 22.9% among men (11).
Although routinely collected clinical data are used for medical research and provide benefits in terms of time, effort, and costs, such data may not be very reliable, especially in the case of India, as it is largely dependent on access to health services and the ability of the people to pay. Moreover, there are several challenges in the use of routine data for specific research purposes.
Several studies have reported the increasing prevalence rates of HT. Although prevalence data have their own merits, they have limitations with respect to chronic conditions such as HT as it is influenced by the duration of the disease. Chronic conditions can persist for years or even decades, and prevalence figures may not reflect changes in disease management, mortality, or treatment effectiveness over time. However, both incidence and prevalence data are useful in policy-making as they help assess the risk and the burden of HT and have their own strengths and limitations.
Given the aging Indian population and huge inequalities in access to health services, which are largely characterized by out-of-pocket expenditure, reliance on routine/prevalence data is likely to provide biased estimates. What would be beneficial to policymakers for planning and implementing preventive strategies is estimating the incidence of new cases of HT. Incident data on HT are currently lacking in many LMICs, including India. In addition, given the increasing burden of HT and CVDs in India, it is necessary to identify the risk factors associated with incident HT. Studies have shown that several risk factors—including aging; rapid urbanization; pre-HT; unhealthy diet; lifestyle changes such as low physical activity, smoking, and alcohol consumption; and an increasing prevalence of obesity and diabetes—are likely to contribute to a rapid rise in HT (12).
Longitudinal studies help identify the development of new cases of HT over time and are more effective in targeting resources for those at risk and implementing preventive strategies at the primary level. A prospective study, namely, the World Health Organization Study on Global Ageing and Adult Health (WHO-SAGE) conducted in two waves (2007 and 2015), provides an excellent opportunity to explore the risk factors associated with the incidence of HT. To the best of our knowledge, there are hardly any studies that have reported incident data on HT and its determinants based on a longitudinal nationally representative data set in the context of LMICs, and India is no exception to this.
Therefore, this study aims to quantify the incidence of HT in adults aged 45 years and older in India and identify the risk factors associated with incident HT. This study not only contributes to the empirical knowledge on incident HT from an LMIC perspective but also has significant implications for health policy in terms of implementing effective preventive strategies at the primary level.
Methods
Study design and participants
The present study used longitudinal data from the Indian sample of the first and second waves of the WHO-SAGE. SAGE is an ongoing, nationally representative longitudinal survey conducted in six LMICs, namely, China, Ghana, India, Mexico, South Africa, and the Russian Federation. Our study focused on individuals who were aged 45 years and older in Wave 2, with baseline individuals aged 37 years and older (due to the 8-year gap between the two waves). The decision to prioritize individuals aged 45 years and older was made with the explicit aim of targeting the aging population as this age cohort is more prone to health issues, including HT. The sample for SAGE India Wave 2 (2015) was the follow-up survey of Wave 1 (2007) in India. The primary purpose of the SAGE India survey was to collect information related to the health and wellbeing of the growing aging population of India.
The survey design of WHO-SAGE incorporated specific primary sampling units (PSUs) and households from the 2003 World Health Survey in India to establish a baseline sample. The survey design covered six Indian states, namely, Karnataka, Assam, Maharashtra, Uttar Pradesh, Rajasthan, and West Bengal. The selection of these states was determined by a combination of factors such as geographical diversity and development indicators such as infant mortality rate, literacy rate of women, percentage of safe deliveries, and per capita income. These states were deliberately chosen to represent various regions and levels of development.
The sampling approaches differed for rural and urban areas. Rural sampling employed a two-stage stratified method, categorizing villages based on household numbers and then employing probability proportional to size sampling for village selection. Each PSU yielded a selection of 25 households. In urban areas, a three-stage approach was used, involving the selection of wards, census enumeration blocks, and households. Cities/towns were grouped into four categories based on the 1991 census population for this purpose (13).
The initial merged sample of Wave 1 and Wave 2 consisted of 3,630 individuals. However, individuals with missing information on any of the variables of interest were excluded from the final data (n = 447). Therefore, our final sample included 3,183 individuals followed in Waves 1 and 2.
Procedures
The blood pressure was measured in both the waves in the right arm/wrist using an OMRON R6 wrist blood pressure monitor using a standard protocol by trained health workers. In this study, the average of the last two readings of the systolic blood pressure (SBP) and the diastolic blood pressure (DBP) was considered for the analysis (14, 15). According to the JNC-7 guidelines, a person was considered hypertensive if he/she had an average SBP ≥140 mmHg or/and an average DBP ≥90 mmHg or was a current user of anti-hypertensive medication at the time of the survey (16). An individual was identified as pre-hypertensive if his/her SBP was 120–139 mmHg and/or if his/her DBP was 80–89 mmHg (16). The 8-year incident cases of HT were defined as those who were free of HT in the first wave but had developed HT by the time the follow-up was conducted. Healthcare utilization was defined as a visit to a healthcare facility as an inpatient or an outpatient at least once during the 12 months prior to the survey.
A set of individual, lifestyle, and household characteristics were included in the analysis to assess the determinants of the incident cases of HT. The individual-level factors were sex (men, women), age group (<45, 45–54, 55–64, 65–74, 75+ years), working status (never worked, not currently working, currently working), marital status (currently married, others), body mass index (BMI) [normal (18.5–24.9 kg/m²), underweight (<18.5 kg/m²), overweight/obese (≥25.0 kg/m2)] (17), stroke (no, yes), diabetes (no, yes), and chronic lung disease (no, yes).
In this study, we grouped the education levels of individuals into four categories, i.e., “no education,” “primary,” “secondary,” and “higher.” These groupings were determined based on the highest formal education level of the individual, as assessed through two questions from the WHO-SAGE India questionnaire. The initial question asked, “Have you ever attended school?” with two possible responses: (1) “yes” and (2) “no.” If an individual had never attended school, they were categorized as having “no education.” Subsequently, a follow-up question inquired, “What is the highest level of education that you have completed?” This question had six possible responses: (1) “less than primary school,” (2) “primary school completed,” (3) “secondary school completed,” (4) “high school (or equivalent) completed,” (5) “college/pre-university/university completed,” and (6) “postgraduate degree completed.” To simplify our analysis, we merged categories (1) “less than primary school” and (2) “primary school completed” into a single category called “primary.” Furthermore, we reclassified category (3) “high school (or equivalent) completed” as “secondary.” Finally, we combined the categories (4) “college/pre-university/university completed” and (5) “postgraduate degree completed” into the “higher” category.
Moreover, the WHO-SAGE Wave-2 questionnaire includes a section dedicated to assessing physical activity, specifically aimed at gathering information regarding activities of moderate and vigorous intensity. Two questions were posed to the respondents, one inquiring about their participation in vigorous-intensity activities that result in significant increases in breathing or heart rate, such as heavy lifting, digging, or chopping wood, and the other inquiring about their engagement in moderate-intensity activities that lead to slight increases in breathing or heart rate, such as brisk walking, carrying light loads, cleaning, cooking, or washing clothes. These questions are designed with binary response options, requiring participants to answer either “yes” or “no.” To classify physical activity, we adopted the criteria proposed by Peltzer and Phaswana-Mafuya (18). Other lifestyle factors included tobacco use (never, former, occasional, current) and alcohol use (no, yes). It may be noted that the prevalence of stroke, diabetes, and chronic lung disease are self-reported.
Wealth quintiles were determined based on household ownership of durable goods and dwelling characteristics. For example, durable goods include factors such as the number of motorbikes or cars and the presence of amenities such as electricity, a television, fixed-line or mobile phone, and a bucket or washing machine. The analysis used for determining the wealth index can be found in the WHO-SAGE India Wave 2 report (13). The household-level characteristics included wealth quintiles (poorest, poorer, middle, richer, richest), caste [scheduled caste (SC)/scheduled tribe (ST), other backward class (OBC), others], religion (Hinduism, Islam, others), and place of residence (urban, rural).
The “caste” reported by an interviewed individual typically falls into one of four main categories: SC, ST, OBC, and “general class.” In India, SC and ST communities are widely recognized as some of the most socioeconomically disadvantaged groups. Conversely, individuals belonging to the general class occupy a higher hierarchical social status. The OBCs, while facing educational, economic, and social challenges, hold a relatively better social standing when compared to the SC and ST categories from a hierarchical perspective.
Statistical analysis
To estimate the incidence rate of HT, new cases that emerged between Waves 1 and 2 of the WHO-SAGE were identified. All non-hypertensives at baseline who were found to have HT in Wave 2 were assumed to have developed HT at the time of follow-up. The incidence rate was then calculated by dividing the number of incident cases by the total number of individuals at the baseline (WHO-SAGE Wave 1) and was expressed per 1,000 people. We provided confidence intervals to address estimation uncertainty. The sample characteristics were expressed as the percentages of the categorical explanatory variables for both men and women participants. The chi-square test was used to compare the distribution of the categories between men and women. Bivariate analysis using Pearson's chi-square test was used to examine the associations of individual, lifestyle, and household characteristics with HT status in Wave 2. Categorical variable (incident HT) changes were analyzed by incorporating various covariates in a binomial logistic regression model. Odds ratios (ORs), 95% confidence intervals (CIs), and p-values were estimated using the generalized estimating equation (GEE) (logit link function) with an exchangeable working correlation matrix and robust standard errors (19). The prevalence of inpatient and outpatient healthcare utilization by HT status was also estimated. The Stata software (version 16.1) was used to execute all the data analysis. A p-value of less than 0.05 was considered statistically significant for all the analyses.
Role of the funding source
The funders of the study had no role in the study design, data collection, data analysis, data interpretation, or the writing of the manuscript.
Results
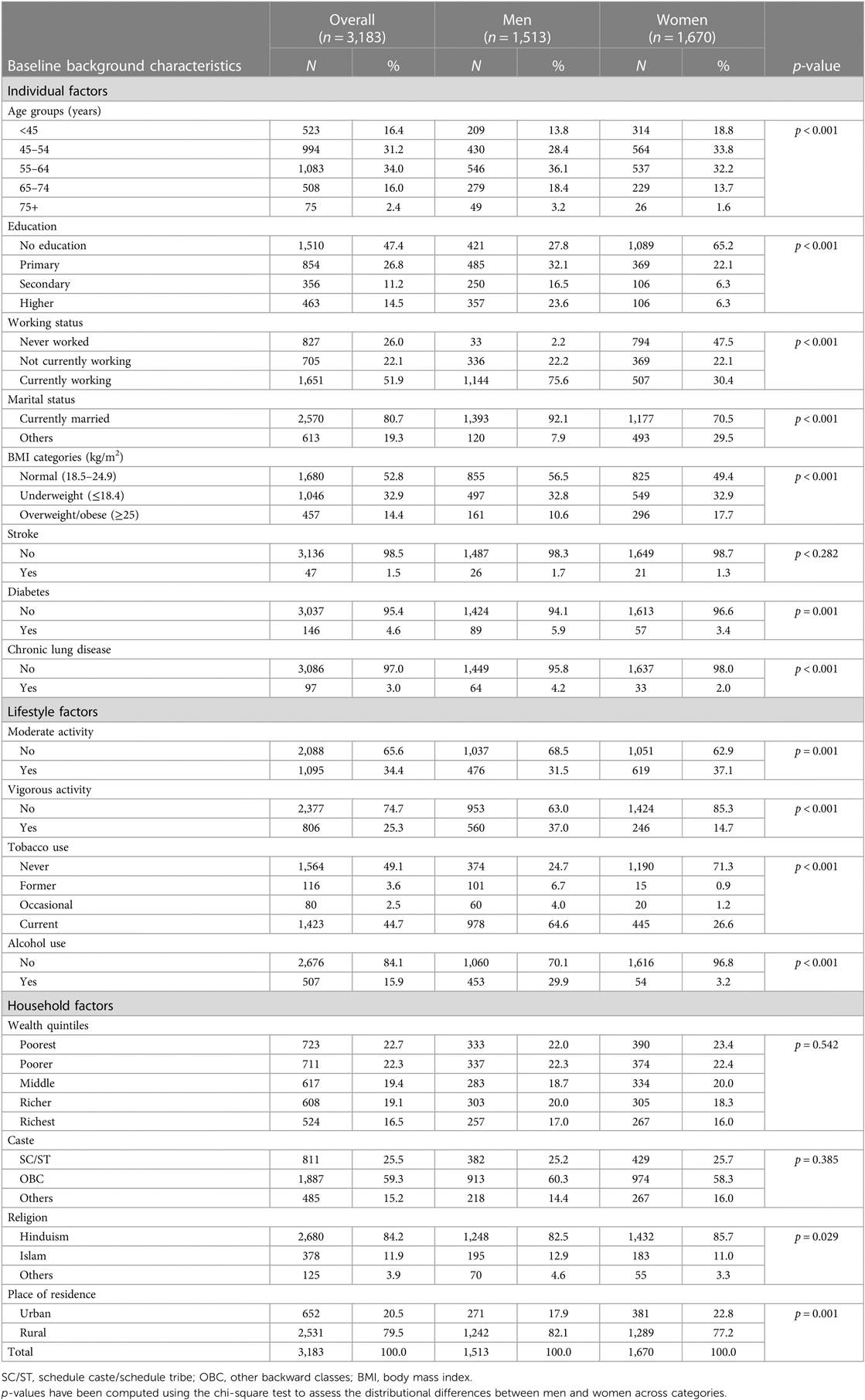
The differences in the sociodemographic characteristics of the included and excluded samples in the study are presented in Supplementary Table S1 (Supplementary Material). The findings indicate that there were no significant disparities between the excluded and included samples in terms of various background attributes, including age group, gender, education, and employment status. Table 1 shows the baseline characteristics and the gender of the overall sample. A total of 3,183 individuals were included in the analysis, of whom 1,513 were men and 1,670 were women. More women than men had no education (65.2% vs. 27.8%), had never worked (47.5% vs. 2.2%), were either unmarried or widowed (29.5% vs. 7.9%), and were overweight/obese (17.7% vs. 10.6%). In contrast, the prevalence of various chronic conditions such as stroke (1.7% vs. 1.3%), diabetes (5.9% vs. 3.4%), and chronic lung disease (4.2% vs. 2.0%) was greater among men than women. Going by lifestyle factors, the prevalence of vigorous activity (37.0% vs. 14.7%), current tobacco use (64.6% vs. 26.6%), and alcohol use (29.9% vs. 3.2%) was higher in men than in women. Nearly 84.2% of the individuals belonged to the Hindu religion, and approximately 79.5% of all individuals were rural residents.
The bivariate analysis of various individual, lifestyle, and household characteristics with the HT status (normal and pre-hypertensive) at the baseline is presented in Table 2. The weighted prevalence of pre-HT at the baseline was 38.2% (unweighted N = 1,086). A greater proportion of pre-hypertensive individuals than normotensive individuals were older, less educated, currently working, and current tobacco users and had a normal body mass index. We did not find any bivariate association of chronic conditions such as stroke, diabetes, and chronic lung disease with HT status.
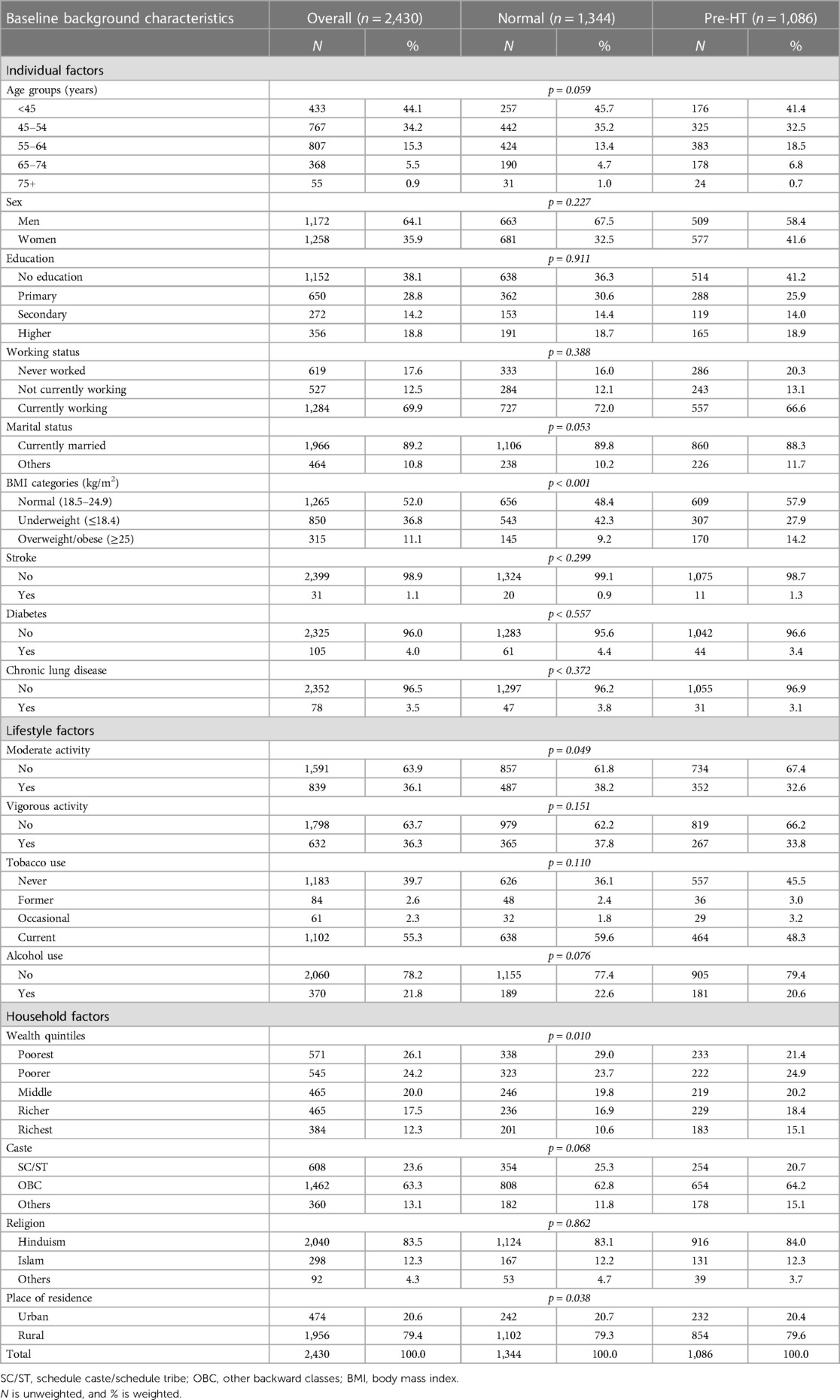
Table 2. Bivariate analysis of hypertension status with various individual, lifestyle, and household characteristics at baseline, WHO-SAGE, India.
Table 3 presents the HT status during the follow-up according to the baseline status of HT. During the follow-up period of 8 years, 31.1% of the pre-hypertensive and 14.4% of the normotensive participants had developed HT. Women had a greater level of conversion from normotension and pre-HT status to HT during the follow-up.
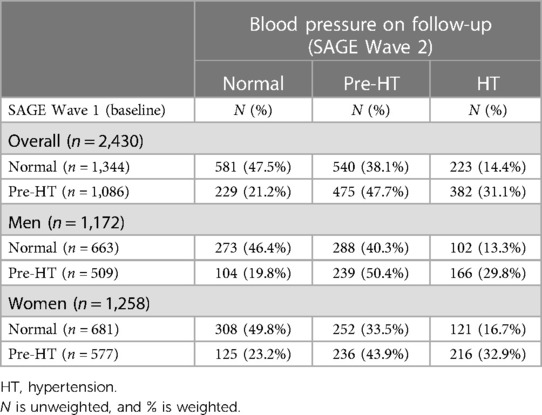
Table 3. The changes in blood pressure category on follow-up according to baseline blood pressure category, WHO-SAGE, India.
The 8-year incidence rates of HT according to the baseline characteristics are presented in Table 4. The 8-year incidence rate of HT was 20.8%. The rate of HT in normotensive and pre-hypertensive individuals was 14.4% and 31.1%, respectively. The incidence rate of HT in normotensive individuals was greater among individuals who were older, women, educated, unmarried or widowed, overweight/obese, moderately active, vigorously active, and alcohol consumers and who had never used tobacco. The incidence rates hold true for HT in pre-hypertensive participants, except for individuals who did not engage in moderate activity or vigorous activity, had a history of tobacco use, or consumed alcohol.
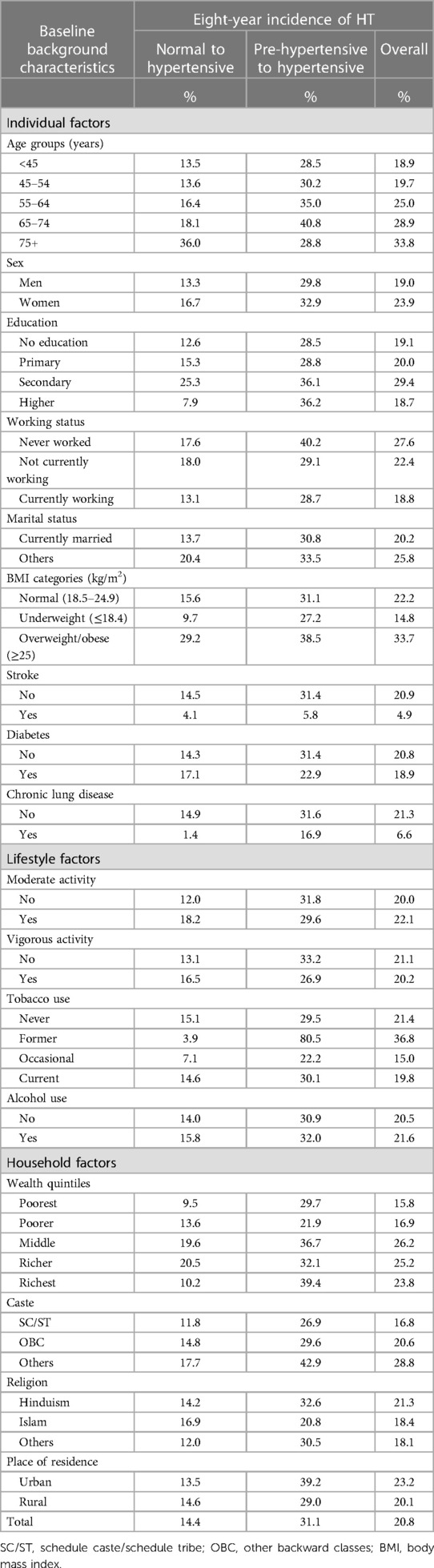
Table 4. Eight-year incidence rates of hypertension (HT) according to baseline blood pressure categories, WHO-SAGE, India.
Table 5 shows the adjusted odds ratio of the incident HT estimated using the GEE (logit link function) according to various individual, lifestyle, and household characteristics. The results suggest that after adjusting for the selected covariates, a greater risk of incidence of HT was observed among the pre-hypertensive participants (OR: 2.24, 95% CI: 1.65–3.03) than the normotensive participants. Similar results were obtained for men and women participants. Wealth status was not significantly associated with the overall incident HT and with incident HT among both men and women participants.
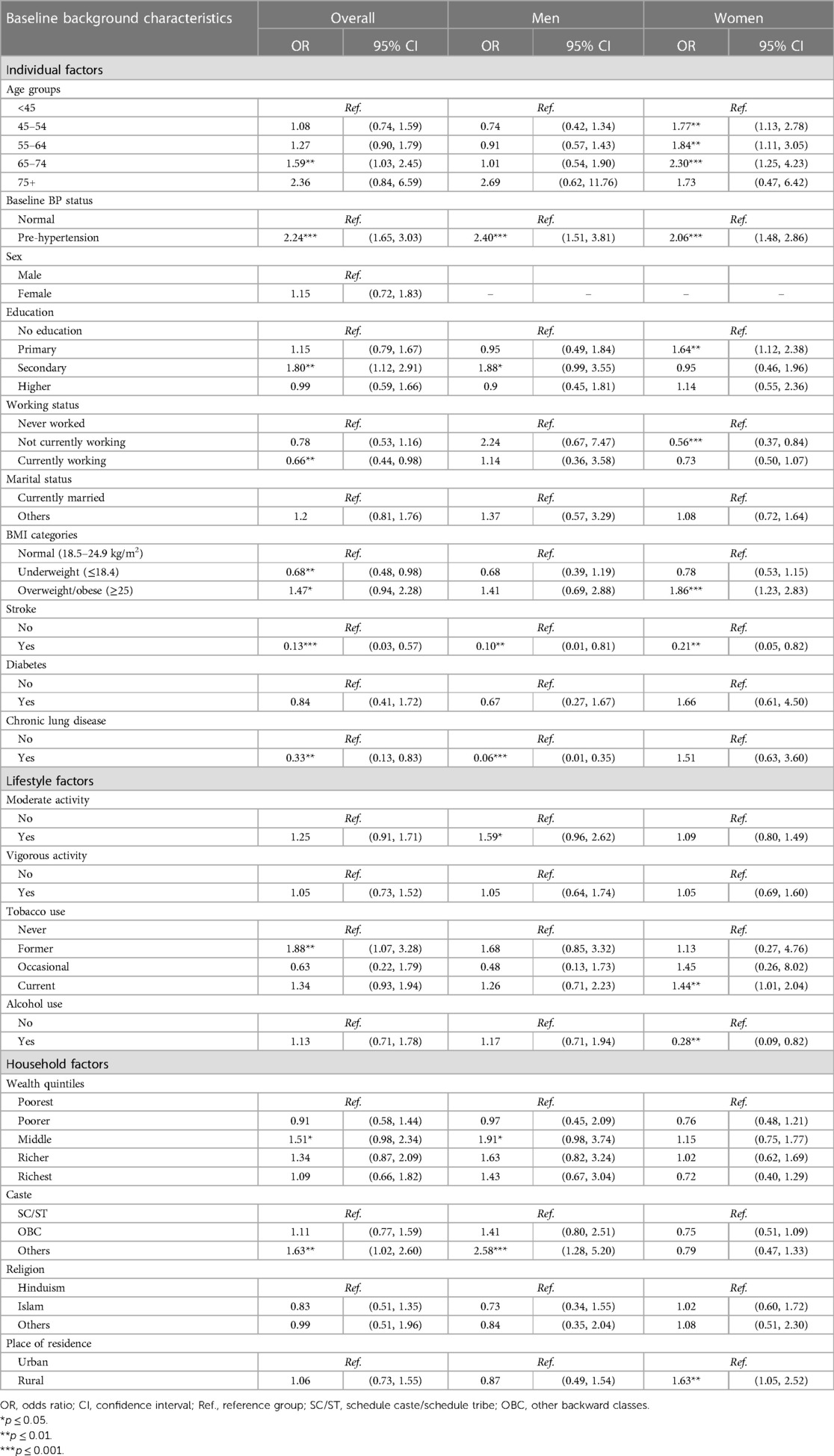
Table 5. Adjusted odds ratio obtained from generalized estimating equation (GEE) with an exchangeable correlation matrix of the incidence of hypertension associated with selected covariates, WHO-SAGE, India.
Discussion
This prospective population-based study estimates incident HT and its determinants. With the increasing burden of CVDs and with HT being a major independent risk factor, health planners and policymakers in India must estimate the incident cases of HT and identify those who are at a higher risk of developing HT in order to target preventive strategies and thus meet public health objectives of reducing the burden of HT and CVDs.
The present study found that during the 8-year period from 2007 to 2015, the incidence of HT in individuals aged 45 years and older was 20.8%, with one in five individuals having developed incident HT during this period. Pre-hypertensive individuals had an overall incidence rate of 31.1 per 1,000 (95% CI: 26.20–35.9), and their risk of developing incident HT was 2.24 odds times higher (95% CI: 1.65–3.03) compared to those who were normotensive. Women who were 45–74 years old, educated up to primary level, overweight/obese, and current tobacco users were more likely to develop HT than their respective counterparts. Similar to other studies, our findings also confirm that age was associated with a higher risk of incident HT among women. Those over 45 years had a significantly higher incidence of HT when compared to those below the age of 45 years among women; however, age was not found to be significantly associated with the incidence of HT in the case of men. Our findings are in line with the earlier findings documented in the literature (20–23).
Very few studies in India have investigated the incidence of HT in the general population, with the reported incidence ranging from 12–34 per 1,000 people (24). A population-based study based on three large cities in South Asia estimated an HT incidence of 9.6 per 100 people in Delhi, 7.6 per 100 people in Chennai, and 7.0 per 100 people in Karachi (25). Studies from countries such as China and South Korea have reported an incidence rate of 53 per 1,000 people (26, 27). A recent population-based cohort study estimated an annual incidence rate of HT of 2.5 per 100 among adults aged 40–65 years in Australia (28). However, caution is advised when comparing results from studies that report incidence rates of HT due to the lack of standardization in terms of age and population considerations, criteria for determining HT, duration of study, etc.
The overall 8-year incidence rate of HT in our study was 20.8% in Indian adults aged 45 years and older. Our findings suggest that pre-hypertensives were at over two times greater risk of developing HT, with a rate of 39 per 1,000 people (95% CI: 32.8–45.0) as compared to normotensive individuals who had a rate of 18 per 1,000 people (95% CI: 13.8–22.3). These results are consistent with several other studies that have reported a greater risk of developing HT among pre-hypertensive individuals (21, 23, 28, 29). However, in contrast to our study, a WHO-SAGE longitudinal study from Ghana reported a reduction in the prevalence of HT (reduction in DBP) over a 12-year period, partly explained by greater awareness of HT among the study participants and increased health insurance coverage over time (30). As observed in our study, a higher incidence of HT among pre-hypertensives may be explained by the higher presence of factors such as higher education, urban residence, obesity, diabetes, use of tobacco, alcohol consumption, and higher wealth quintile status among them as compared to those with normal HT. High incident rates of HT among pre-hypertensives, coupled with aging, increasing obesity, and high prevalence of diabetes, are a major cause for concern for policymakers as this cocktail is likely to increase the prevalence of HT and CVD mortality and morbidity in India.
To achieve the target of a 25% relative reduction in HT by 2025, the Government of India has launched the India Hypertension Control Initiative (IHCI). The guidelines on HT screening in India include both opportunistic screening and targeted screening. Opportunistic screening is recommended for those over 18 years of age at every contact with the health system, including with community health workers. On the other hand, targeted screening for HT is aimed at detecting HT among high-risk populations at the community level (31).
The results obtained from our study can be extremely useful in guiding effective interventions among pre-hypertensives who are at higher risk of developing HT. There is sufficient evidence that screening for HT does provide health benefits, especially among high-risk adults (32, 33). In addition to routine and opportunistic screening, early prevention of HT is possible by identification of pre-hypertensives, through strategies such as targeted screening, thus reducing the risk of developing HT. Similarly, prompt treatment of pre-hypertensives can be initiated for those who develop HT. The implications of our findings for both primary and secondary levels of prevention are obvious and are likely to minimize complications and adverse outcomes associated with untreated HT. In addition, the importance of monitoring particularly those with pre-HT cannot be overemphasized. As there are no current guidelines specifically on pre-HT in India (34), it is recommended that guidelines specific to pre-HT are developed and acted upon, with necessary training imparted to the front-line staff.
This approach aims to mitigate the risk of high BP and, subsequently, the risk of CVDs in this population as there is evidence to suggest that controlling BP can avert one-third of CVD mortality (34). Unfortunately, given the huge income inequalities, high out-of-pocket payments, weak government health services, unaffordability of private-sector health services, and lack of pre-HT screening guidelines, it is inevitable that a significant proportion of pre-hypertensives and those at risk of incident HT will remain undiagnosed and will be missed out by the health system. Even among those identified as hypertensives, there are concerns regarding initiation of treatment and compliance to treatment, given the issues around affordability of anti-hypertensive drugs as they are to be purchased through out-of-pocket payments from private pharmacies.
Studies have shown that the treatment rate of HT in India is only 44.0% (35). In the absence of effective monitoring and follow-up, even those who have initiated treatment are less likely to have their blood pressure under control. Again, studies have shown that the control rate of HT in India is 10.4% (35). With high out-of-pocket payments and the predicted rise in incident HT, the economic burden of HT and CVDs on households and its impact on the health systems could be significant.
It may also be noted that the association of risk factors of HT has commonly been reported in prevalence studies but not from incident data. Unlike other cross-sectional studies which provide estimates for a single point in time, the strength of our study is that it uses longitudinal data and reports incident data and risk factors from a prospective perspective. This study therefore contributes to the empirical knowledge of incident HT literature from an LMIC context. Although this is a strength of our study, there are also certain limitations to it. These include the small sample size, restricting the generalizability of the study findings, and the long follow-up of over 8 years, resulting in loss to follow-up. Although the BP measurement was taken multiple times, this was undertaken on a single visit, which may affect the reliability of the research findings by overestimating the incidence of HT (36). In addition, information on comorbidities such as stroke, diabetes, and chronic lung disease, treatment seeking, etc., is self-reported and may have been open to recall bias since memory limitations of the participants may have led to underreported health conditions and may have skewed medical history and lifestyle factors, affecting research reliability. In addition, we did not attempt to differentiate recall bias, if any, between comparison groups. Lastly, the study did not include biometric measures such as triglycerides, cholesterol, and uric acid to assess their impact on the incidence of HT.
Conclusion
This prospective population-based study conducted in India reveals a worrisome incidence rate of HT among individuals aged 45 and older, with one in five people having developed HT over an 8-year period. Pre-hypertensive individuals face more than twice the risk of HT compared to normotensive individuals, while factors such as lower educational levels, overweight/obesity, and older age exacerbate this risk. Women are particularly vulnerable. The study emphasizes the urgent need for targeted preventive strategies, including opportunistic screening of pre-hypertensives and other high-risk individuals. Although the guidelines on HT screening in India do include both opportunistic screening and targeted screening, challenges within the healthcare system in India, such as income disparities and limited access to affordable treatment, pose significant obstacles to effective HT management. It is recommended that effective implementation of screening programs, both at the point of health service utilization and at the community level, to detect pre-HT and initiate necessary treatment, would be a cost-effective approach to address the growing burden of HT and associated CVDs in India.
Data availability statement
Publicly available datasets were analyzed in this study. These data can be found here: https://www.iipsindia.ac.in/content/Lasi-wave-i.
Ethics statement
The study underwent review and approval by the World Health Organization's Ethics Review Board in Geneva, Switzerland, and the Institutional Review Board of the International Institute of Population Science in Mumbai, India. The survey agencies that conducted the field survey for the data collection have collected prior informed consent (written and verbal) from the respondents.
Author contributions
MB: Conceptualization, Funding acquisition, Writing – original draft, Writing – review & editing. PD: Conceptualization, Writing – original draft, Writing – review & editing. MK: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. LKD: Conceptualization, Data curation, Formal Analysis, Methodology, Writing – review and editing.
Funding
The authors declare financial support was received for the research, authorship, and/or publication of this article.
This research received funding from the LSE Covid Impact Fund for Research and Knowledge Exchange.
Acknowledgments
We are extremely grateful to the two anonymous reviewers for their comments and suggestions that have improved the quality of the revised manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2023.1265371/full#supplementary-material
References
1. World Health Organization. Fact sheet on noncommunicable diseases. New York City, New York: World Health Organization (2021). Available at: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (Accessed March 24, 2023).
2. Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. (2016) 134(6):441–50. doi: 10.1161/CIRCULATIONAHA.115.018912
3. James MF, Dyer RA, Rayner B. A modern look at hypertension and anaesthesia. Southern Afr J Anaesth Analg. (2011) 17(2):168–73. doi: 10.1080/22201173.2011.10872770
4. Luo X, Yang H, He Z, Wang S, Li C, Chen T. Numbers and mortality risk of hypertensive patients with or without elevated body mass index in China. Int J Environ Res Public Health. (2021) 19(1):116. doi: 10.3390/ijerph19010116
5. Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990–2015. JAMA. (2017) 317(2):165–82. doi: 10.1001/jama.2016.19043
6. United Nations. Department of economic and social affairs. Policy brief no 153. India overtakes China as the world's most populous country. New York City, New York: United Nations Department of Economic and Social Affairs (UN DESA) (2023). Available at: https://www.un.org/development/desa/dpad/wp-content/uploads/sites/45/PB153.pdf (Accessed March 18, 2023).
7. Ministry of Health & Family Welfare, Government of India. Standard treatment guidelines. Hypertension: screening, diagnosis, assessment, and management of primary hypertension in adults in India. New Delhi, India: Ministry of Health and Family Welfare, Government of India (2016).
8. UNFPA. Policy brief | Harnessing India's demographic dividend. New Delhi, India: UNFPA India (2018). Available at: https://india.unfpa.org/en/publications/policy-brief-harnessing-indias-demographic-dividend (Accessed February 26, 2023).
9. Koya SF, Pilakkadavath Z, Chandran P, Wilson T, Kuriakose S, Akbar SK, et al. Hypertension control rate in India: systematic review and meta-analysis of population-level non-interventional studies, 2001–2022. Lancet Reg Health Southeast Asia. (2023) 9:100113. doi: 10.1016/j.lansea.2022.100113
10. Gupta R. Trends in hypertension epidemiology in India. J Hum Hypertens. (2004) 18:73–8. doi: 10.1038/sj.jhh.1001633
11. Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. (2005) 365(9455):217–23. doi: 10.1016/S0140-6736(05)17741-1
12. Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. (2020) 16(4):223–37. doi: 10.1038/s41581-019-0244-2
13. Arokiasamy P, Parasuraman S, Sekher TV, Lhungdim H. Study on global ageing and adult health (SAGE) wave 2, India national report. International Institute for Population Sciences Geneva: World Health Organization (2020).
14. Wohlfahrt P, Cífková R, Movsisyan N, Kunzová Š, Lešovský J, Homolka M, et al. Threshold for diagnosing hypertension by automated office blood pressure using random sample population data. J Hypertens. (2016) 34(11):2180–6. doi: 10.1097/HJH.0000000000001076
15. Jose A P, Awasthi A, Kondal D, Kapoor M, Roy A, Prabhakaran D. Impact of repeated blood pressure measurement on blood pressure categorization in a population-based study from India. J Hum Hypertens. (2019) 33(8):594–601. doi: 10.1038/s41371-019-0200-4
16. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. (2003) 42(6):1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2
17. World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. (2000) 894:i–xii, 1–253.11234459
18. Peltzer K, Phaswana-Mafuya N. Fruit and vegetable intake and associated factors in older adults in South Africa. Glob Health Action. (2012) 5:1–8. doi: 10.3402/gha.v5i0.18668
19. Sathish T, Kannan S, Sarma SP, Razum O, Sauzet O, Thankappan KR. Seven-year longitudinal change in risk factors for non-communicable diseases in rural Kerala, India: the WHO STEPS approach. PLoS One. (2017) 12(6):e0178949. doi: 10.1371/journal.pone.0178949
20. Dannenberg AL, Garrison RJ, Kannel WB. Incidence of hypertension in the Framingham study. Am J Public Health. (1988) 78(6):676–9. doi: 10.2105/AJPH.78.6.676
21. Diederichs C, Neuhauser H. The incidence of hypertension and its risk factors in the German adult population: results from the German National Health Interview and Examination Survey 1998 and the German Health Interview and Examination Survey for Adults 2008–2011. J Hypertens. (2017) 35(2):250–8. doi: 10.1097/HJH.0000000000001151
22. Ahn K-S, Park S-K, Cho Y-C. Risk factors for hypertension of middle aged male workers using data from health check-ups. J Korea Acad Ind Coop Soc. (2012) 13(10):4686–93. doi: 10.5762/KAIS.2012.13.10.4686
23. Sathish T, Kannan S, Sarma P, Razum O, Thankappan K. Incidence of hypertension and its risk factors in rural Kerala, India: a community-based cohort study. Public Health. (2012) 126(1):25–32. doi: 10.1016/j.puhe.2011.11.002
24. Anchala R, Kannuri NK, Pant H, Khan H, Franco OH, Di Angelantonio E, et al. Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. (2014) 32(6):1170–7. doi: 10.1097/HJH.0000000000000146
25. Gupta P, Singh K, Shivashankar R, Singh K, Vamadevan A, Mohan V, et al. Healthcare utilisation and expenditure patterns for cardio-metabolic diseases in South Asian cities: the CARRS study. BMJ Open. (2020) 10:e036317. doi: 10.1136/bmjopen-2019-036317
26. Liang Y, Liu R, Du S, Qiu C. Trends in incidence of hypertension in Chinese adults, 1991–2009: the China health and nutrition survey. Int J Cardiol. (2014) 175(1):96–101. doi: 10.1016/j.ijcard.2014.04.258
27. Lee JH, Yang DH, Park HS, Cho Y, Jun JE, Park WH, et al. Incidence of hypertension in Korea: 5-year follow-up study. J Korean Med Sci. (2011) 26(10):1286–92. doi: 10.3346/jkms.2011.26.10.1286
28. Nguyen B, Bauman A, Ding D. Association between lifestyle risk factors and incident hypertension among middle-aged and older Australians. Prev Med. (2019) 118:73–80. doi: 10.1016/j.ypmed.2018.10.007
29. Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D. Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: a cohort study. Lancet. (2001) 358(9294):1682–6. doi: 10.1016/S0140-6736(01)06710-1
30. Menyanu EK, Corso B, Minicuci N, Rocco I, Russell JC, Ware LJ, et al. Determinants of change in blood pressure in Ghana: longitudinal data from WHO-SAGE waves 1–3. PLoS One. (2021) 16(1):e0244807. doi: 10.1371/journal.pone.0244807
31. Ministry of Health and Family Welfare. Screening, diagnosis, assessment, and management of primary hypertension in adults in India. New Delhi, India: Government of India (2016).
32. Schmidt BM, Durao S, Toews I, Bavuma CM, Hohlfeld A, Nury E, et al. Screening strategies for hypertension. Cochrane Database Syst Rev. (2020) 5(5):CD013212. doi: 10.1002/14651858.CD013212.pub2
33. US Preventive Services Task Force, Krist AH, Davidson KW, Mangione CM, Cabana M, Caughey AB, et al. Screening for hypertension in adults: US Preventive Services Task Force reaffirmation recommendation statement. JAMA. (2021) 325(16):1650–6. doi: 10.1001/jama.2021.4987
34. World Health Organization. India hypertension control initiative, a high impact and low-cost solution. New Delhi, India: World Health Organization (WHO) (2022). Available at: https://www.who.int/india/news/detail/02-06-2022-india-hypertension-control-initiative–a-high-impact-and-low-cost-solution (Accessed July 2022).
35. Bhatia M, Kumar M, Dixit P, Dwivedi LK. Diagnosis and treatment of hypertension among people aged 45 years and over in India: a sub-national analysis of the variation in performance of Indian states. Front Public Health. (2021) 9:766458. doi: 10.3389/fpubh.2021.766458
Keywords: incident hypertension, longitudinal study, pre-hypertension, adults aged 45 years and older, WHO-SAGE, India
Citation: Bhatia M, Dixit P, Kumar M and Dwivedi LK (2023) A longitudinal study of incident hypertension and its determinants in Indian adults aged 45 years and older: evidence from nationally representative WHO-SAGE study (2007–2015). Front. Cardiovasc. Med. 10:1265371. doi: 10.3389/fcvm.2023.1265371
Received: 22 July 2023; Accepted: 20 October 2023;
Published: 14 November 2023.
Edited by:
Serafino Fazio, Federico II University Hospital, ItalyReviewed by:
William Kofi Bosu, West African Health Organisation, Burkina FasoRofingatul Mubasyiroh, National Research and Innovation Agency (BRIN), Indonesia
© 2023 Bhatia, Dixit, Kumar and Dwivedi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mrigesh Bhatia m.r.bhatia@lse.ac.uk
 Mrigesh Bhatia
Mrigesh Bhatia Priyanka Dixit
Priyanka Dixit Manish Kumar
Manish Kumar Laxmi Kant Dwivedi
Laxmi Kant Dwivedi